- Find a Doctor
- Services & Specialties
-
-
Services & Specialties
-
-
-
-
- Find a Location
-
-
Find a Location
More than 100 independent, locally owned locations in neighborhoods across the state of Washington. Explore our:
-
-
-
-
- News & Resources
-
-
News & Resources
- Welcome Our Newest Doctors
- Latest News
- Learn More About Our Surgery Centers
- Why Proliance Surgeons?
- Meet Our Leadership
- Meet Our Board
- Contact Us Today
- Pay My Bill
- Career Opportunities
- Mission, Vision, Values
- Phreesia FAQ
- Insurance Plans
- Medical Records
- Balance Billing Protection Act
- PELTO Health Partners
- Revenue Cycle Credit Resolution
- Proliance Surgeons Foundation
-
-
-
-
- Pricing
Exceptional outcomes
personally delivered
every day

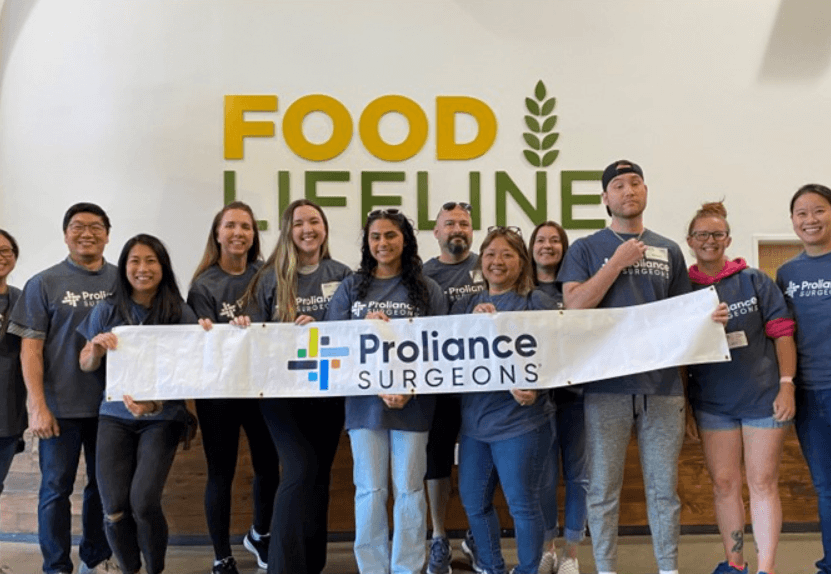
Volunteer with Food Lifeline to Support Our Communities
Saturday, April 20, 2024
1:00 PM - 3:00 PM
Volunteer with us on a team adventure! We will be volunteering at Food Lifeline in South Seattle. Let’s come together, sort, and repack nutritious food for individuals and communities experiencing hunger.
1:00 PM - 3:00 PM
Volunteer with us on a team adventure! We will be volunteering at Food Lifeline in South Seattle. Let’s come together, sort, and repack nutritious food for individuals and communities experiencing hunger.
Exceptional Outcomes
Personally Delivered.
As an independent group of specialists and surgeons, we have been helping the people of Washington get healthy, and stay that way, for 20 years. We understand each care need is unique, and that’s why we give you choices in care delivery. After all, your healing process is personal, and the best treatment starts by getting to know you as a person, not just a patient.
Proliance Surgeons by the Numbers
0
+
Providers
We’re each dedicated to specific areas of care.
1:1
Care Experience
We know each care need is unique, and we treat you that way.
0
Average Rating
We’ve earned high satisfaction ratings from our patients.
Specialty care, right in your neighborhood
Complete care near you
With over 100 care centers, surgery centers, therapy clinics, imaging centers, and urgent care, we can support you close to home.
Trending Topics

Services & Specialties
Ambulatory Surgery Centers Provide Choices for Faster Recovery
Ambulatory Surgery Centers are an alternative to hospitals for outpatient surgery. They often have faster...

Resource
Improved Patient Safety During COVID-19
Proliance Surgeons is focused on patient safety as our highest priority. Our surgeons and management...

Resource
Why Proliance Surgeons?
From hip surgery to midwifery, there are so many reasons to choose Proliance Surgeons.