During pregnancy, stretching of the abdominal muscles is common.
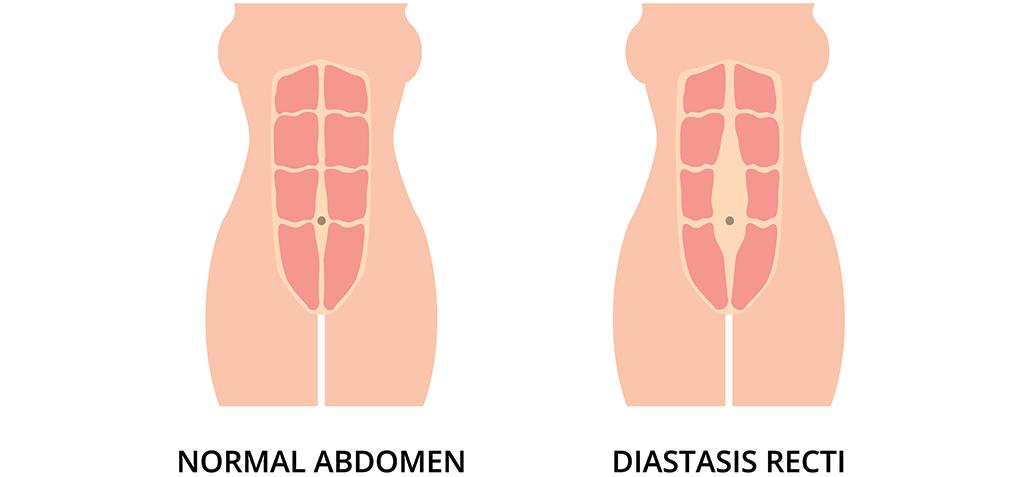
We all have fibers (called fascia) that provide structural integrity to our abdominal wall. The fascia surrounds the mid-abdominal rectus abdominus muscles (think, the 6-pack area of your stomach). Ideally after childbirth, your fascia should return to pre-pregnancy state.
However, it’s important to note not all bodies achieve this result. In fact, about 60% of post-pregnancy women are diagnosed with diastasis recti following pregnancy, and while it’s not the only cause of this diagnosis, it’s a prevalent one.
Diastasis recti is the medical term for excessive stretch of the abdominal tissues, causing damage to the fascia that give your abdominal wall structural strength.
Some women, especially petite women who have large babies, find that their fascia fibers have been too far stretched to return to normal state. Accordingly, the rectus muscles may stay extremely thinned out or become lateralized on each side. There are differing degrees of diastasis – most women have mild degrees of diastasis with little impact, but for some, the resulting long-term loss of core strength can be significant.
What are the Symptoms?
Women with significant diastasis recti say that they are always consciously holding their abdomen “in” by engaging their rectus muscles, and when they relax, the abdomen protrudes as if they were 4-6 months pregnant. The tension this creates on the edges of the muscles can cause pain, especially by the end of the day.
Additionally, the lack of structural support of the anterior abdominal wall can result in lower back pain over time. Many women find it impossible to develop core strength, which is well-understood to be important in overall health.
Patients with diastasis can also experience pelvic floor muscle spasms. It’s important to note that pelvic floor issues will likely not resolve with diastasis repair, so separate management is recommended. If you are having pelvic floor muscle spasms, consult with a Urogynecologists who specializes in the pelvic floor.
If you are experiencing the symptoms above, your provider will conduct a physical examination to further understand the cause behind your symptoms. In my practice, we examine for a weakness of tissues of the middle of the abdomen centered at the belly button when laying down on your back. When the rectus muscles are tensed or engaged, the weakness of the middle of the abdomen allows pressing into the abdomen, as well as definition of the edge of the muscles giving an estimate of the width of the muscle separation.
Is it Diastasis Recti or a Hernia?
It is necessary to distinguish symptomatic diastasis recti from typical hernias. In the case of a typical hernia, there is an actual tear in the fascia and the internal fat or even bowel/intestine can protrude out, in danger of becoming “stuck” or “incarcerated.” The blood supply to the bowel may become compromised, leading to bowel “strangulation.”
In the case of diastasis, there is a severe stretch, but no tear in the fascia. Accordingly, there isn’t a danger of bowel incarceration or strangulation.
Unfortunately, women are typically told that because there is no danger of bowel incarceration or strangulation, there is no need to worry about their symptoms, and no treatment for diastasis.
In my opinion, when diastasis is severe, the symptoms of pain and functional impact on activities of life make it similar to a large ventral hernia. Depending on the severity of symptoms and examination findings, I offer patients abdominal wall reconstruction.
Abdominal Wall Reconstruction:
What is it?
Abdominal wall reconstruction involves removal of the stretched out, thin mid-abdominal fascia, placing the muscles back to the midline, and reinforcing the midline with mesh (synthetic) or biologic matrix (a sheet of specially prepared biologic tissue) to prevent breakdown and strengthen the area. This procedure can be performed with or without a tummy tuck (abdominoplasty) depending on the degree of redundancy of the skin and soft tissue of the mid and lower abdomen. Abdominal wall reconstruction is typically covered by insurance; however, the tummy tuck component usually is not.
The goal of abdominal wall reconstruction is to address abdominal wall pain symptoms related to symptomatic diastasis recti, but also to return the patient to a functional abdominal wall. We aim to restore anterior abdominal wall integrity and to allow core strengthening and exercise potential, with optimal overall health in mind.
What isn’t it?
It’s important to note, that the abdominal wall reconstruction should be distinguished from a tummy tuck or abdominoplasty. The abdominoplasty portion is usually a separate cost that insurance does not cover.
Some women turn to plastic surgery for their diastasis recti condition. Plastic surgeons focus on the skin and underlying fatty layer and sometimes will imbricate (cinch-up) the fascia. They may even use overlay mesh reinforcement, but they do not excise the weakened fascia or place the muscles back to their midline position with underlying reinforcement as with abdominal wall reconstruction.
Additional Considerations:
- Abdominal wall reconstruction for diastasis recti is not commonly offered by general surgeons, so you will need to do some research around your residence.
- It’s necessary to be certain you are not planning to become pregnant again.
- The abdominal wall reconstruction surgery is usually a 2.5 – 4-hour operation and requires a 2 – 3-day hospitalization.
- There are temporary drainage tubes that remain for 10 – 14-days, and by two weeks most women are off narcotic pain medications.
- By one-month patients feel back to normal, and at 8 weeks you are allowed to begin exercising the abdomen and working on re-establishing core strength.
- For mild or moderate diastasis recti, physical therapy can be a helpful treatment, and should be a consideration for initial management before surgery is considered.
In Summary:
If you are experiencing the symptoms of diastasis recti, it’s important to find the right care provider who can fully assess your symptoms and provide sound direction for your future. And if appropriate, abdominal wall reconstruction may be the solution you need to relieve pain and return to an active lifestyle. Re-establishing your core strength is an opportunity to create lifelong impact on your health.